With the dawn of COVID-19 (coronavirus), many of us have likely heard about “telehealth” or “telemedicine.” So, what exactly is it? Put simply, telemedicine is any kind of long distance communication of medical information. There are several types of telemedicine, and they encompass everything from video chatting with your provider to doctors directing patients on how to track their own symptoms at home. In asynchronous, or “store-and-forward” telemedicine, data is collected from the patient and passed on to a specialist in a different location. All kinds of medical care can be performed via telemedicine, including dentistry, radiology, dermatology, ophthalmology, and, of course, psychiatry. Telepsychiatry, what we practice at Free Range Psychiatry, is a specific kind of telemedicine that covers many of the things a psychiatrist may normally offer their patients including evaluations, managing medications, and therapy.

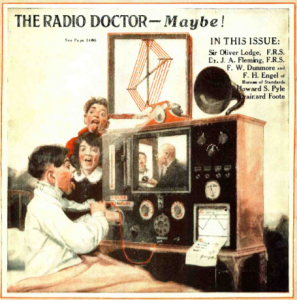
Early imaginations of telemedicine as seen on the February 1925 cover of Science and Invention (Science and Invention magazine)
How does telemedicine actually work? Though some providers opt for voice-only conversations, most prefer to video chat with their patients. So, you’ll need access to a device with a camera, speaker, and microphone – this is generally a computer, but a smartphone can often get the job done just as well. Healthcare providers will typically send patients a link or specific instructions to access the site they utilize. Sometimes this is done through versatile sites like Zoom, and other times more specialized sites such as TeleHealth are used. As a patient, you’ll follow the link or log into the website and have a virtual chat with your doctor. Easy peasy. From here, the process is essentially the same as an in-person office visit, except this time you’ll simply close the browser window and return to your activities at home instead of walking out of the office and driving home. It is important to keep in mind that with all telemedicine, but specifically with telepsychiatry, patients are encouraged to be mindful of the space in which they log in for the appointment. This should be a quiet, private room in which the patient feels safe to speak as openly with their provider as they would in the office.
It seems like telemedicine has come out of the wood work during this pandemic in many ways. However, it has actually been around for quite awhile. One could argue that it began as early as ancient times when smoke signals were used to communicate plague outbreaks, depending on how strict your definition of telemedicine is. As with all modes of communication, telemedicine has evolved over time with new developments in technology, some even being initially driven for NASA and military use. In the mid 1920s, doctors began using radio to communicate with their patients. The idea of remote medicine was clearly on many minds as two separate magazines, Science and Invention and Radio News, ran issues with covers showing a doctor diagnosing a patient through a radio and television. Little did they know that they had essentially predicted telemedicine as we commonly know it today. Since then, the internet has proved to be an enormously impactful invention for telemedicine and has enabled doctors to do things that previously only existed in dreams, or magazine covers.
A doctor examines a patient remotely on the cover of the April 1924 issue of Radio News (Radio News Magazine)
Across its different modes and subfields, telemedicine has shown to be just as effective as in-person care, and to even have some significant benefits. For example, being able to send pathology slides of a virus or CT scans of a head injury to a specialist in a different location than the patient can lead to a more accurate diagnosis and therefore a better outcome for the patient. It also allows patients in rural areas to be connected with the healthcare they need and would otherwise be too far away from to reasonably access. Telemedicine can even lead to some notable cost reductions for both patients and providers. Studies have shown that telepsychiatry in particular is reliable and on par with in-person equivalents.
With COVID-19 and the introduction of social distancing, suddenly a much larger portion of the population was in need of remote medicine. Unsurprisingly, telemedicine use increased dramatically as a result. The entire world was thrown into an environment in which we need to be as creative as possible on how to provide the service that people need while maintaining the space necessary to keep everyone safe, and telemedicine was there to answer the call. It has allowed providers to continue to work with their patients at a distance, and has also aided in streamlining the process of in-person care by pre-screening patients, minimizing contact between patients and providers in hospitals, and even using algorithms to factor in local COVID-19 data when determining treatment plans.

At this point, most of us are very familiar with the mental toll that a global pandemic can have on an individual. From the constant overhead of worry about family members and the general state of the things, to the sudden absence of “normal” activities like going to work or out for a drink with friends, we have all likely felt some decline in our well-being. As a result of this and the policy changes put into action, telepsychiatry specifically has seen a rise during this pandemic. At Free Range Psychiatry, telepsychiatry has always been our primary mode of providing care and this has only been further affirmed by COVID-19. We feel grateful to have already had the tools in place to continue our work as we had been when so many other practitioners were forced to make significant changes to their practice. Without telemedicine technology, we would not be able to do what we do and we are glad to see it making a difference in so many lives.






Leave A Comment